You might have heard about pelvic floor therapy (sometimes called pelvic rehab) online or from a fellow mom, but what is it? Who needs it? Where do you find it? And what should you expect? We dive into all things pelvic-y in this month’s blog.
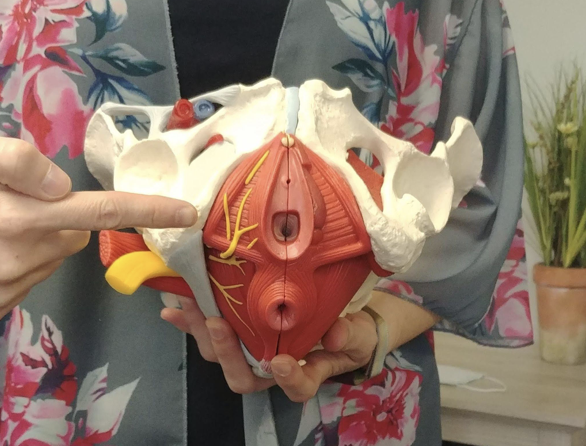
“Pelvic floor therapy is a specialized kind of therapy to relieve the symptoms of pelvic floor dysfunction”….yeah, yeah…anyone can google and find that on webmd.com, but what does it mean? Okay, ladies and gentlemen let’s get down to the nitty gritty. There are a lot of muscles that attach to your pelvis (think hip muscles, core muscles, leg muscles as well as the pelvic floor muscles), and any of these muscles could start to bother you. In particular, the muscles of the pelvic floor could begin to give you trouble. These are small but powerful muscles that have a lot of jobs to do.
-
They prevent all our organs from falling through our pelvis.
-
They allow us to pee and poo when we want to (and if they aren’t working right – this is a problem!).
-
They relax and contract to let us have and enjoy penetrative vaginal intercourse and orgasms.
-
They stabilize the whole pelvis from the bottom. They are like the foundation of your core.
So pelvic floor therapy deals with these muscles as well any muscle that attaches to the pelvis and any complaints that someone might have in these areas.
Some common reasons people come to pelvic floor therapy are:
Incontinence (even the loss of just a few drops of urine with cough and sneeze isn’t supposed to happen)
Pelvic Pain (this could be endometriosis, coccyx pain, vulvodynia, hip pain, SIJ pain, pain with sitting or with moving)
Pain with Intercourse
Pregnancy prep
Postpartum care
DRA (Diastasis Rectus Abdominis)
Lets dive into each one of these a little bit to see why they happen and why a therapist trained in movement and muscles is the right person to help you. Skip around to the section that best describes you!
Incontinence
This could be bladder or bowel leakage, but bladder is certainly more common. There are many reasons why incontinence could be happening, but the most common would be that the muscles aren’t working right in the pelvic floor. There are specific muscles to stop you from urinating and muscles to stop you from having a bowel movement. If these muscles are too weak they can cause you to leak, but if they are too tight they can cause you to leak too! I know what you are thinking, because I hear it all the time. “Wait? Wouldn’t tight muscles be a good thing to stop me from peeing?” Think of it like a stiff neck. If your neck muscles are stiff and tight you would have a hard time responding and moving your head quickly. The same could be true for the pelvic floor muscles. And isn’t that what we are asking our pelvic floor muscles to do when we cough or sneeze? We are asking them to turn on really fast and strong. Like that stiff neck, they just can’t move quickly enough for us. Other reasons you could be leaking might be posture and hip weakness. Some studies have shown that poor posture and hip weakness could also cause or worsen incontinence.
As you can see, a lot goes into keeping you dry, and pelvic floor therapy helps to assess all the muscles and the way they function to help determine what might be causing you to drop a drop or two when you don’t want to.
Pelvic Pain
Certainly, pelvic pain can be the most debilitating condition we pelvic floor therapists see. It can range from just pain during your period to constant pain for years. And there are soooo many things that can cause pelvic pain. Some common things that I see are tight muscles (imagine walking around with your fist clenched all day – it would be aching like mad!), weak muscles, scar tissue, nerve compression or irritation, and poor alignment. A skilled pelvic floor therapist is able to test out the muscles, nerves, pelvic alignment and scar mobility and give you a thorough assessment as to why and how they are contributing to your pain. Then you work hand-in-hand with your therapist to learn to overcome and treat each and every condition that is found on your examination.
Pain with intercourse
What a frustrating experience dyspareunia (that’s the fancy word for ‘pain with intercourse’) is! You tell your partner you want to have penetrative vaginal intercourse, your body is telling you that it wants it, and then something comes near the vaginal canal or enters it and there is pain! After a number of times trying, you might even give up, or you might be too scared to try to have sex because of the pain. Why does this happen? Sometimes pain can arise due to a lubrication issue and trying a lubricant should be one of the first things to try. But, in my experience, pain with intercourse is most often due to muscle guarding, muscle tightness, or scar tissue.
So dyspareunia is treated very similarly to pelvic pain. We teach you how to relax your muscles. We do hands on releasing and stretching exercises and then discuss options like dilators if needed.
Pregnancy Prep and Postpartum Care
Pregnancy is one of the most taxing and challenging natural experiences you can put a human body through. You are gaining significant weight, shifting organs, growing organs, growing a human life, stretching skin and muscles of the abdomen during pregnancy and, then stretching skin and muscles of the pelvic floor during labor and delivery. And all these changes happen FAST! The onslaught of hormones and weight changes can cause a lot of different feelings in the body that may include back pain, pelvic pain, and bladder troubles. Pelvic floor therapy is a great way to help guide you through the changes, limit pain, and limit future troubles. I often recommend a session early on in pregnancy to discuss how the body will change and how to keep yourself moving and grooving with as little pain as possible. Then, near the end of pregnancy, it’s a great idea to come in and discuss positions and strategies during labor and delivery tailored specifically to your body and your birth plan, to help you have a safe and successful birth. You can even do a session of pushing practice where, through the use of ultrasound, you can literally see what is happening in your pelvis when you try to push. Up to 30% of new moms don’t realize they are actually tightening their pelvic floor muscles instead of relaxing them during labor, and that can slow things down a little bit.
After delivery, we recommend a checkup around that 6-10 week time period similar to your checkup with your provider. This checkup is to see how well your muscles are turning back on and coming back into the right position. We see if there is a significant diastasis rectus abdominis (we’ll talk about this more in a moment), if your abdominal muscles are turning back on like they should, and, if your pelvic floor muscles are healing. If you are still having any lingering pain or incontinence, we’ll dive into why that is happening and what to do to get you back on track. And if there is an activity (like running) you want to get back to, we discuss how to gradually return to exercise and your favorite activity. This is a great supplement to your regular postpartum provider checkup and, I believe, a must-have for all moms. It’s just another way to make sure you are healing well in the postpartum period.
DRA (Diastasis Rectus Abdominis)
So this is when the ‘six pack muscles’ in the front of your abdomen get stretched apart. Some will call it an abdominal separation. Now, please moms, understand that up to 100% of pregnant people have this condition at the end of their pregnancy! It is normal and natural to have some degree of separation of the abdominals. There is simply so much abdominal stretching that occurs during pregnancy that it is rare to not have some separation. However, these muscles should quickly come back together in the postpartum period. If the muscles aren’t coming back together or you are noticing a doming in the abdomen when you try to use your abs (maybe when you are getting into and out of bed you’ll notice it), this is a sign that you could use some help to rehab the core. When you see a well-trained pelvic therapist for this condition, they will work on manual techniques to return the muscles to the normal position, as well as training you how to get your abdominal muscles firing properly to keep you safe and strong. This type of therapy can help limit back pain and pelvic pain as well.
So who needs pelvic floor therapy? Well, I’m a little biased since I am a pelvic floor physical therapist, but I’d say anyone who owns a pelvis could probably benefit from therapy. But particularly anyone who has any of the above complaints or conditions could benefit from pelvic floor therapy! It isn’t scary or weird (okay, maybe a little different than any physical therapist you may have seen in the past but this is a pretty important part of your body that you really want working properly), and all my patients are so glad that they took the time to care for themselves and their pelvis.
What can you expect from pelvic floor therapy? Therapy at Adore Your Core Physical Therapy begins with a thorough discussion of your medical history, birth history and surgical history. We discuss what complaints you know you have as well as dive into, and ask about,areas you might not have thought about (like bladder and bowel stuff). Once we know a little more about you, we can start a physical assessment. This varies a little depending on what you are coming in for, but in general we see how you move and how strong you are, and then tailor the exam to your chief complaints. We are looking to assess the nerves, muscles, and body alignment in order to find out how they might be causing or affecting your complaint. So, for example, if your complaint is DRA then we will do a thorough assessment of the core. If you have other complaints like pain with intercourse or urinary incontinence, we may recommend an internal pelvic exam in order to assess the pelvic floor muscles. Typically, the best way to assess the pelvic floor muscles is through a vaginal or rectal examination but this isn’t set in stone and if you aren’t comfortable or don’t want an internal exam it doesn’t have to happen. The internal exam is really patient dependent. It is based on the patient’s comfort level and their complaints. After a thorough examination, we discuss each of your concerns. We’ll talk about what seems to be causing this complaint, and in what ways we will address and fix the problem in therapy. The evaluation is finished up with a few exercises, stretches, or other education to start you on your path to recovery. Then we make subsequent appointments to get into any treatment that needs to be done. Typically patients are seen four to eight times over the course of a few months, but this also varies widely depending on what they are coming in for and how quickly they respond to therapy. You are always in charge of your therapy, and we discuss your goals and how you want to achieve them.
Now that I’ve gotten everyone super excited about pelvic floor therapy (insert a chuckle here), I’m sure you’re wondering where you can find a therapist. A true pelvic floor therapist has taken, at a minimum, nearly a hundred hours of additional training to be able to specialize in this area. These therapists are highly trained and are not your run-of-the-mill physical therapists or occupational therapists. You want to make sure that the person you pick has been trained in this area and is comfortable with and performs internal examinations (even if you don’t plan to have an internal examination, asking this question will give you an idea of whether the person truly is a well-trained therapist). If you are in the Western New York area, Adore Your Core Physical Therapy is a private clinic dealing only in this type of therapy. You can also find therapists using a locator, such as www.pelvicrehab.com or https://pelvicguru.com/directory/ to try and locate therapists.
I hope you have enjoyed this month’s blog on pelvic floor therapy and are feeling much more informed about your pelvis and its many jobs. Be happy and stay well!
Author Racquel Kurzweg, PT DPT is a Doctor of Physical Therapy, is the owner of Adore Your Core Physical Therapy. Previously, she developed pelvic floor physical therapy programs at two different clinics within a local hospital system, as well as creating an inpatient program for new mothers to receive physical therapy in the hospital after birth. She has also been a part of teaching childbirth education classes, postpartum fitness classes and public speaking events to small and large audiences on incontinence and pelvic health.